NCH&C recognised for the quality of its preceptorships
NCH&C accredited for the quality of its preceptorships

NCH&C is delighted to have received the National Preceptorship Interim Quality Mark.
The National Preceptorship Programme was established in November 2021 to design, develop and deliver a Preceptorship Framework for Nursing for England and associated quality standards for all health and social care organisations.
Representatives from NHS England and the Norfolk & Waveney Integrated Care Board attended Norwich Community Hospital to present NCH&C with an award recognising the quality of our preceptorships.
Carolyn Fowler, Director of Nursing & Quality at NCH&C, received the award on behalf of NCH&C from Geraldine Rodgers OBE, Director of Nursing, Leadership & Quality at NHS England & Improvement.


For newly-qualified nurses, nursing associates and AHPs, preceptorship is an important part of their career journey. Preceptorship is a more structured approach to the first year of practice after graduation. To help ease into the transition of clinical work, during this first year clinicians are given extra support and on-the-job training. This ensures all healthcare professionals are working to the high standards we need, and setting them up for success in the rest of their career. Visit the NHS England website to find out more about preceptorships in the NHS and why they matter.
Following a thorough assessment, NCH&C was successfully awarded the National Preceptorship Interim Quality Mark. The assessing panel was particularly impressed with NCH&C’s Multi-Professional Preceptorship Policy and Preceptorship Handbook were excellent, they also stated that our Preceptorship Portfolio Workbook was ‘exemplary’.
Lynne Fanning, Head of Clinical Education and Research at NCH&C, expressed her delight with the new award:
“Preceptorship is important for us at NCH&C more so now, than ever. We are delighted to be awarded the Interim National Preceptorship for Nursing Quality mark for our work on the development of a Multi-Disciplinary policy and programme to support our preceptors and preceptees, following the newly published National guidance for AHPs and Nursing staff. The purpose of preceptorship is to provide support, guidance and development for all newly-registered practitioners to build confidence and develop full competence as they transition to autonomous professionals (National Preceptorship Programme, 2022) and we are committed to ensure that all of our preceptees are given the opportunities for support and development as they move into what may be their first post in the NHS”.
Carolyn Fowler, Director of Nursing & Quality at NCH&C, also shared her gratitude to the teams who made this recognition possible:
“I am so delighted that NCH&C has been recognised for the support we offer to colleagues who are on preceptorship. Continual learning is vital for the development of our workforce, so it is essential that all those on preceptorship are well-supported. A big thank you to NCH&C’s Clinical Education team for their continual support of our learners, and their commitment to this particular piece of work.”
A big thank you to everyone who supports our wonderful preceptees, and who helped make this accreditation possible.

Upcoming recruitment events for NCH&C
Find out more about working in Norfolk's community NHS

Interested in a healthcare career but want to find out more?
Perhaps you’re not sure if you have the qualifications required for one of our entry-level roles, or maybe you have a few questions about returning to clinical practice after a career break?
We know the job-seeking process can be a bit daunting and off-putting, so we want to make it easy as possible for you to find a new career you love. If you have any questions at all about working at NCH&C, come along to one of our friendly and informal recruitment open days to find out more.
You can find us at the following recruitment events…
- 17 April 2024 – Job Centre Plus Careers Event, Norwich Job Centre, Castle Quarter
- 15 May 2024 – Job Centre Plus Careers Event, Norwich Job Centre, Castle Quarter
- 20 May 2024 – 50+ Jobs Fair, Dereham Job Centre
- 7 June 2024 – Watton Jobs Fair, Queens Hall, Watton
- 25 June 2024 – Armed Forces Jobs Fair, Dereham Job Centre
- 24 July 2024 – Jobs Fair Norwich, The Forum
Our experienced Career Development team will be on hand at all these events to answer your questions. They can even support you with your application, and provide guidance on how to prepare for your interview.
If you have any questions, please contact careerdevelopment@nchc.nhs.uk
We’ll be sharing details of more of our Norfolk recruitment events very soon!
NCH&C nurse and research fellow to present pathway at international conference.
Anca Manea, NCH&C Community Learning Disability Nurse and NICHE Research Fellow, is set to present her ground breaking project addressing the sustainability of the Norfolk Antenatal Pathway for Women and Birthing People with Learning Disabilities at a prestigious international conference in August of this year.
The NICHE, or Norfolk Initiative for Coastal and Rural Health Equalities, Fellowship has been funded by Health Education England (East of England) to support Norfolk and Waveney Integrated Care System to co-create projects that will help to recruit, develop and retain the health and social care workforce and improve services to meet the needs of the local communities it serves.
Intended to enhance antenatal care for individuals with learning disabilities, Anca will present to the International Association for the Scientific Study of Intellectual and Developmental Disabilities (IASSIDD) Conference in Chicago, in August this year.
Speaking on the announcement, Anca commented: “Last year I was awarded a NICHE Fellowship that I am using to explore the sustainability of the Norfolk Antenatal Pathway for Women and Birthing People with Learning Disabilities. This project was initiated by NCH&C and has been joined by other significant stakeholders within Norfolk, with the purpose of enhancing antenatal care for individuals with learning disabilities. I am incredibly proud to be presenting the Pathway, and representing NCH&C, at the IASSIDD Conference in Chicago, later this year.”
NCH&C are very proud to have our own dedicated research team who work across all our services to support the delivery of NIHR research projects.
Stay up to date with their work by visiting our website.
Striving for a Neuro-inclusive Health Service
Striving for a Neuro-inclusive Health Service
Diversity and inclusion have become increasingly talked about over recent years. These discussions have spanned industries, including sports, commercial, education and obviously, healthcare. This Neurodiversity Celebration Week, Lauren Britcher, Occupational Therapist, and Dr Stephanie Summers, Clinical Psychologist and Clinical Lead, in the NCH&C Neurodevelopmental Service, share tips on how healthcare workers can better support individuals who are Neurodivergent.
Neurodiversity is an umbrella term that includes a range of Neurodivergent conditions including Autism (ASD), Attention Deficit Hyperactivity Disorder (ADHD), Dyspraxia, Dyscalculia, Dyslexia, and Tourette’s Syndrome.
The Equality Act (2010) says that reasonable adjustments should be made for individuals with ASD and ADHD (an official diagnosis is not required), to ensure they are not substantially disadvantaged when accessing services such as education, employment, and health care. ASD and ADHD are registered disabilities and therefore it is a legal requirement to provide reasonable adjustments to support individuals to access a range of activities including education, employment, and health care services.
Within the UK there is a strong Neurodivergent community that re-frames neurodiversity as a difference with brain development that can bring many strengths. They highlight that it is environments, and lack of understanding, that can result in these differences disabling people with ASD/ADHD from participating alongside the rest of their community. This is a valid reminder for services, employers, and the education system to consider if what they are providing is neuro inclusive. Within the Neurodevelopment Service (NDS) at NCH&C we work with a range of children, young people, and their families through their ASD/ADHD assessments. As a team we are constantly reflecting on and adapting our service to make our approach more neuro-inclusive; not only for the individuals we support but for the staff working in NDS too.
What can healthcare workers do to better understand and support individuals who are Neurodivergent?
Be Person-Centred
- Ask the patient what support they need, what would be helpful when attending appointments and delivering care to them?
- Consider speaking with people who know your patient best (with their consent of course) – what can they tell you about how to support the patient? What do they use at home with that person in their everyday life?
- Remember, even though lots of individuals have the same diagnosis, everyone is different in their strengths and needs.
Make Reasonable Adjustments
Adjusting your services to help individuals who are Neurodivergent access health care is essential. This may include:
- Use of neuro-inclusive communication – have a range of ways to share information, including easy read version of leaflets/letters, social stories of what to expect coming to and during appointments and use of visuals rather than text. Providing information discussed in appointments in a written format can aid memory and understanding.
- Offering appointments via face-to-face, phone call or video call for people to choose what suits them. Can you use questionnaires to reduce conversation, as this is an area some individuals find difficult?
- Some Neurodivergent individuals can find attending healthcare appointments a very uncomfortable experience. Consider the sensory experience of the environment – is it noisy? Lots of visual stimulation? Bright lights? Uncomfortable/rough chairs? Is there anything you can do to reduce the impact of these? Think about consistency, can they see the same clinician in the same room/space? This can help people know what to expect when attending appointments and in turn reduces anxiety.
Don’t Forget Your Colleagues!
Many people you work with in your team may also be neurodivergent. Therefore, improving your knowledge and understanding will also help them in their daily lives at work.
There are some great resources from the Royal College of Nursing (RCN) about supporting neurodivergent nursing colleagues. However, these concepts can be applied to all NHS staff.
Lauren Britcher, Occupational Therapist
Dr Stephanie Summers, Clinical Psychologist and Clinical Lead
Neurodevelopmental Service, NCH&C
Click here for more information about how we’re marking Neurodiversity Celebration Week.
Neurodiversity Celebration Week, 18-24 March
Neurodiversity Celebration Week 18-24 March 2024
Neurodiversity Celebration Week is a global initiative, which challenges stereotypes and misconceptions about neurological differences. It aims to transform how neurodivergent individuals are perceived and supported, while creating more inclusive and equitable cultures that celebrate differences and empower every individual.
What is Neurodiversity?
Neurodiversity is about recognising that everyone’s brain works differently. Everyone will have their own unique way of thinking, interacting, and experiencing the world. Neurodiversity is based on the concept that neurological variances should be recognised and respected just like any other human variation, such as gender, race, or sexual orientation.
Examples of Neurodiversity include:
- Autistic Spectrum Disorder (ASD)
- Attention Deficit Hyperactivity Disorder (ADHD)
- Dyslexia
- Developmental Coordination Disorder (DCD) or Dyspraxia
- Dyscalculia
- Developmental Language Disorder
- Tic Disorders, including Tourette’s Syndrome
- Intellectual Disability
Laura Clear, Deputy CEO and Executive sponsor the Diverse Abilities Staff Network, NCH&C, says: “Our people make NCH&C who we are, and it is important that we properly support anyone with a Neurodiversity – whether a staff member, a patient, or carer.
“Neurodiversity Celebration Week is an opportunity for us all to learn a bit more about the different ways our brains work and is a good reminder of the importance of kindness and acceptance. People’s abilities are varied, and everyone is different. As an organisation, we recognise and value those differences.”
We encourage you to use this week to learn more about the different types of Neurodiversity and the ways in which you can support your colleagues and our service users.
Attend a Neurodiversity Celebration Week event
There is an official schedule of events taking place throughout the week, including panel discussions with inspirational speakers from a range of backgrounds and professions. We would encourage staff to attend any events of interest.
We want to use this week to focus on how we provide support to our staff and how we are supporting our service users.
There will be stalls taking place in our reception areas during the week. Please feel free to stop by and ask any questions:
| Date | Location and Time |
| Monday 18 March | NCH Reception, 11am – 2.30pm |
| Thursday 21 March | Attleborough Reception, 11am – 2.30pm |
| Friday 22 March | North Walsham Reception, 11am – 2.30pm |
Visit the Neurodiversity Celebration Week website for more information.
NCH&C is a top performing community trust in the NHS Staff Survey 2023
NCH&C is a top performing community trust in the NHS Staff Survey 2023
Last year we invited all our staff to complete the National NHS Staff Survey 2023. One of the world’s largest workforce surveys, and the best way for our staff to share their views about their job, our organisation, and the NHS.
63% of our substantive staff responded to the survey – that’s 1,567 people. For the second year, bank-only workers were also invited to complete the survey, of which 25% did.
The results are now live, and some highlights include:
- Results showed that we were the top performing community trust for staff recommending NCH&C as a place to work
- NCH&C was one of the top performing community trusts for the theme “We work flexibly” and for the sub-theme “Support for work-life balance”
- 8 in 10 people feel their manager takes a positive interest in their health and wellbeing
- 8 in 10 people feel the people they work with are understanding and kind to one another
- 8 in 10 people feel they are able to make suggestions to improve the work of their team / department
- 8 in 10 people would be happy with the standard of care provided by this organisation for a friend or relative
These positive themes were also reflected in the responses of our Bank staff:
- 7 in 10 bank workers look forward to coming to work
- 7 in 10 choose to work as a bank worker in the NHS because of the flexible working arrangements, and 9 in 10 agree they can decide the hours and shift patterns they want to work
- 9 in 10 bank workers feel that their role makes a difference to patients
- 9 in 10 bank workers feel they receive the respect they deserve from colleagues
Overall, the areas where the trust is reporting successes is centred on autonomy and our people feeling freedom within their role to decide how to work, and the ability to make suggestions to improve where they work. Success in these areas has led to the trust being one of the best performing community trusts for staff recommending NCH&C as a place to work.
NCH&C’s CEO, Matthew Winn, said:
“I’d like to thank everyone who took the time to complete the NHS Staff Survey. All services and staff are continuing to work under huge pressure and despite this their commitment to delivering great community health and care support shines through.
“The wellbeing of our staff is our priority, and I am pleased that the work the trust has done over the past 12 months is reflected in improvements in these results in supporting our staffs’ ability to work flexibility. NCH&C is now one of the best performing community trusts for supporting work-life balance, and in the overall People Promise element: ‘We work flexibly’.
“The survey gives us clear feedback on areas where we need to make further progress including relationship building with both colleagues and managers, burnout, and inclusion. We will be addressing these areas of concern to ensure improvements are made and the right level of support is implemented throughout the trust.”
Results can be viewed in full, here:
Ensuring our diverse workforce feel engaged, included, and heard
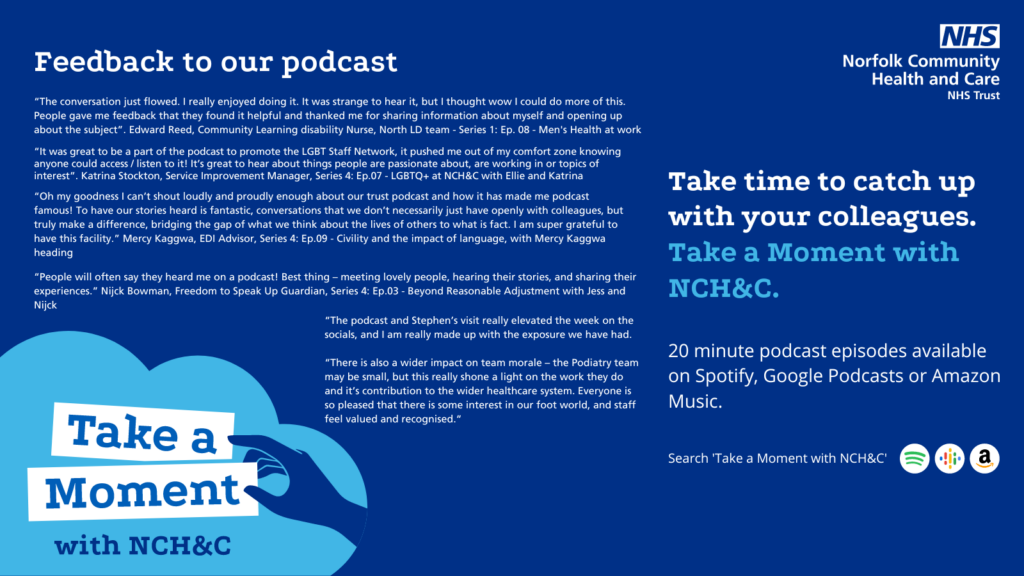
Take a moment with NCH&C
NCH&C introduced ‘Take a Moment with NCH&C’ podcasts in 2022, a sector leading and transformative communication approach.
Since then we have covered personal and insightful stories from a wide variety of people on an array of subjects. This includes carers, menopause, men’s health, LGBTQ+ personal stories, reasonable adjustments, and baby loss. Have a look at all our podcasts and listen here.
Almost 100 episodes of the podcast have been published to date with almost 10000 downloads. Its presence on platforms like Spotify and Amazon Music ensures a broad audience reach beyond internal staff. To further enhance its scope and impact, the podcast is planned, created, and published by a communications team that actively pursues potential interviewees and collaborations while fostering staff engagement through volunteer storytelling.
Earlier this year our podcast was awarded ‘Highly Commended’ at the Employers Network for Equality and Inclusion (ENEI) Inclusivity Excellence Awards.
In a case study about ‘Take a moment with NCH&C’, the ENEI said: “The podcast’s impact transcends numerical data, evident in its effectiveness as a communication tool and recruitment magnet.”
“In the first half of 2023, podcast-related social media posts reached 18,686 unique viewers, indicating significant interest, and driving traffic to NCH&C’s profile, a positive sign for recruitment efforts. Additionally, the podcast serves as a potent tool for potential recruits to gauge the organisation’s support and respect for its staff, fostering recruitment of a diverse workforce.”
Vicky Brooke, NCH&C’s Head of Communications, Marketing, and Engagement, said: “Official recognition for our podcast from the ENEI as an effective and regarded channel of communication is amazing. Staff tell us that they’ve listened to the 100 episodes we’ve so far created with genuine interest. It’s provided a great way to build empathy and understanding across our community trust and beyond.
“Right now we’re looking at the next phase for NCH&C’s podcast, including the possibility of creating department and service-specific episodes to further enrich the podcast’s value inside and outside of the organisation. We’re excited about launching a new series for the podcast in mid 2024.”
Celebrating Overseas NHS Workers’ Day 2024
Celebrating over overseas NHS colleagues

Friday 1 March 2024 is Overseas NHS Workers’ Day.
Since its launch over 75 years ago, overseas healthcare professionals have played a vital role in the history of the NHS.
Of course, overseas workers have impacted healthcare long before the NHS existed. From pioneers such as Annie Brewster who emigrated from St Vincent in the 1860s and became known the Nurse Ophthalmic treating a variety of eye conditions in Whitechapel Hospital (now know as the Royal London), to James Samuel Risien Russell who is recorded as the first Black British consultant specialising in neurology in the 1880s and subsequently setting up his own mental health practice in the 1900s.
To support colleagues who identify as being an ‘overseas worker’, NCH&C recently launched its Global Unity Wellbeing Group. An informal sub-group of our Diverse Heritage Staff Network, the Global Unity Group is a supportive community for internationally recruited colleagues, or those who were educated overseas. This welcoming group is a place for internationally educated staff to meet in-person, network and get to know each other, participate in bespoke learning opportunities, and celebrate the diverse heritage of our growing workforce. The launch event back in November saw new and established staff come together to enjoy food, including an introduction to “chips and gravy!”

My Story: Paschal Okorie
This Overseas NHS Workers’ Day, one of our internationally educated colleagues, Paschal Okorie, agreed to tell us their story.
Paschal is a Physiotherapist based in West Norfolk. Here is their story…
“In the words of Roy Bennett’s ‘The light in the heart’, it is said that no one has ever achieved greatness without dreams. Also, Walt Disney in one of his famous quotes posited that if you can dream it, you can do it.
“The idea of studying physiotherapy came when I was a little younger. Due to my love for football (watching and playing) and general wellbeing of people, having accompanied my mother to the hospital as she used to take my little brother who at the time was diagnosed with congenital talipes equinovarus (club foot). Also, watching football and seeing how the physios and the doctors will run into the field to help players when they are injured grew my passion.
“In 2010, I gained admission into the university to study my dream course (Medical Rehabilitation) for 5 years and graduated in September 2015 with Bachelor of Medical Rehabilitation (Physiotherapy) degree. I also proceeded to get my practising license in March 2016 and the rest, as they say, is history.
“As someone who is keen to keep adding more knowledge and would love to keep progressing in the profession – and who loves to travel to learn new things, especially other people’s culture, I applied for HCPC license in 2021 in other to migrate to the UK despite the pandemic at the time. I finally got registered with HCPC and by January 2022, I got a job role offer for a Band 6 Physiotherapist at NCH&C, after working in my home country for 5 years post induction.
“I would say so far that the journey has been smooth, and I have settled quickly into my new role and environment, despite the pressure of coming to a different country and trying to acclimatise with the environment, people, and culture, and the new job role, working to do my best to improve the service when called upon, and providing high quality care for patients.
“It’s been a roller coaster of multiple experiences from adapting to use of SystmOne, engaging in data transfer to ITP, replying to emails and tasks on daily basis, team meetings etc. and combining this with attending to my rota daily. All thanks to a great MSK West team members ably led by Sarah Hogan who have been very supportive and accommodating. I would like to specially appreciate Elinor who was the first person to welcome me to King’s Lynn out of her busy schedule at Norwich in the absence of my line manager at the time. I want to appreciate Richard for releasing his bicycle to help me get to work on time from QEH quarters. I would like to also appreciate Jamie, Frank, Chioma, Tracy, Clare, and Sara for the various roles they played in making sure I did settle in without much difficulty.
Finally, the journey just began.”
To find out more about Equality, Diversity & Inclusion at NCH&C, please visit our We Care microsite.
Willow Therapy Unit Recruitment Open Day
Complete an application and have an interview on the day!

NHS recruitment open day for healthcare jobseekers – complete an application and have an interview on the day!
Norfolk Community Health & Care NHS Trust (NCH&C) is holding a recruitment open day for healthcare professionals, and those who want to get started on their healthcare career journey.
Friday 23 February
09:30 – 16:00
The King’s Centre, Norwich, NR1 1PH
The informal drop-in event is for anyone who wants to find out more about working at NCH&C’s new Willow Therapy Unit. Attendees will also be supported to complete job applications in person, and complete interviews on the day if they wish.
Opening in Spring 2024, the Willow Therapy Unit will be a start-of-the-art new therapy unit based at Norwich Community Hospital on Bowthorpe Road. Staff will use cutting-edge technology and the latest therapeutic practices to help patients get strong enough to return home, following a stay in acute hospital. The new unit will be an important resource for helping the people of Norfolk stay well and in their own homes.
NCH&C is hiring for a range of roles at the new Willow Therapy Unit, including Nurses, Physiotherapists, and Occupational Therapists, as well as unregistered roles like Assistant Practitioners and Clinical Support Workers – perfect for individuals just starting out in their healthcare career journey. NCH&C welcomes applications from newly qualified clinicians, and those whose professional registrations may have lapsed. In both cases, NCH&C can support individuals as they gain confidence and competence in relevant clinical skills.
Kate Pontin, Operational Director for Transformation & Delivery at NCH&C, offered a warm invitation to anyone interested in a new healthcare career:
“We know the job-hunting process can be daunting, especially if you are at the start of your career or returning to work after a break, so we want to remove as many obstacles as possible with our upcoming recruitment open day at the King’s Centre. Anyone who’s interested in pursing a healthcare career is encouraged to come along to find out more.
“NCH&C colleagues will be on-hand to answer any questions about the new Willow Therapy Unit, and support attendees to complete job applications where needed. We know interviews can be particularly nerve-wracking, so we’ll be offering informal, ‘getting to know you’ interviews on the day, too, for those who want them. It’s also a chance to find out more about working at NCH&C. We pride ourselves on being a rewarding place to work, where staff can make a real difference every day as part of an amazing team. We also prioritise autonomy and staff wellbeing, with free gyms, access to a staff wellbeing service, free physiotherapy, and regular refreshments”.
Willow Therapy Unit will be one of ten inpatient units operated by NCH&C in Norfolk. Operating across the whole of Norfolk, NCH&C’s 2,500 staff also delivers health and care in the community, including in patients’ homes, care homes, and GP surgeries.
For more information about working at Willow Therapy Unit, click here.
NCH&C celebrates We Care Day on 14 February
NCH&C celebrates We Care Day on 14 February
On Wednesday 14 February we’re celebrating NCH&C’s 3rd annual We Care Day. A day dedicated to championing our staff, encouraging allyship within our staff networks, and creating a sense of belonging across the organisation. We Care Day supports and celebrates the many cultures that make up NCH&C.
NCH&C has three staff networks: Diverse Abilities, Diverse Heritage, and LGBTQ+. These networks provide staff with a safe place to share stories, work together to create inclusive policies, and offer peer-to-peer learning and development.
Staff are further supported by our two new wellbeing groups which support staff who are further impacted by the communities that they intersect. Our Global Unity Wellbeing Group supports our internationally educated staff members, and our Staff Carers Wellbeing Group support our staff who are also carers outside of work.
NCH&C recognises the need to provide a safe environment for our staff to be authentically themselves and gain the support they need to be successful in their roles. We Care Day was launched to promote our staff networks and raise the sense of belonging across the organisation.
In the year since we last celebrated, we have:
- Created two new wellbeing groups: Global Unity and Staff Carers
- Welcomed Liz Cooke, Director of HR and OD, as our Executive Sponsor for the Diverse Heritage We Care Staff Network
- Won a silver ‘excellence in inclusion award’ for our staff lived experience conversations via the ‘Take a Moment with NCH&C’ podcast
- Maintained Disability Confident Leader status for the fourth year running
- Hosted our first in-person staff network meeting for LGBTQ+ members
- Became a Veteran Aware Bronze Award member organisation
- Set-up an anti-racist workplace committee
The We Care initiative is a unifying symbol of allyship. This We Care day, think about how you can show others support and care: check-in on a colleague, host a We Care Event (email wecareevents@nchc.nhs.uk for more info), or become a staff network ally.
